Answer: The best supplements for lowering cortisol, supported by clinical research, are ashwagandha (particularly KSM-66 or Sensoril extracts), magnesium glycinate, and high-dose omega-3 fatty acids (EPA/DHA). These agents work through distinct mechanisms: ashwagandha modulates the stress-response system, magnesium supports enzymatic cortisol regulation, and omega-3s reduce stress-induced inflammation. Effective daily doses are 250-600 mg for ashwagandha, 200-400 mg for magnesium glycinate, and 1-2.5 g for combined EPA/DHA. They are most effective when used strategically over 8-12 weeks alongside foundational lifestyle practices and under professional guidance.
Thank you for reading this post, don’t forget to subscribe!For those navigating chronic stress, the promise of a “cortisol-balancing” supplement can be alluring. Yet, the path from marketing claims to measurable, physiological change requires navigating a complex landscape of biochemistry and evidence. This guide moves beyond basic lists to examine the specific mechanisms, clinical dosing, and strategic protocols for the most research-backed supplements. We focus on creating a synergistic, personalized approach that respects the body’s innate rhythms and the principle that supplements are supportive tools, not substitutes for a healthy foundation.
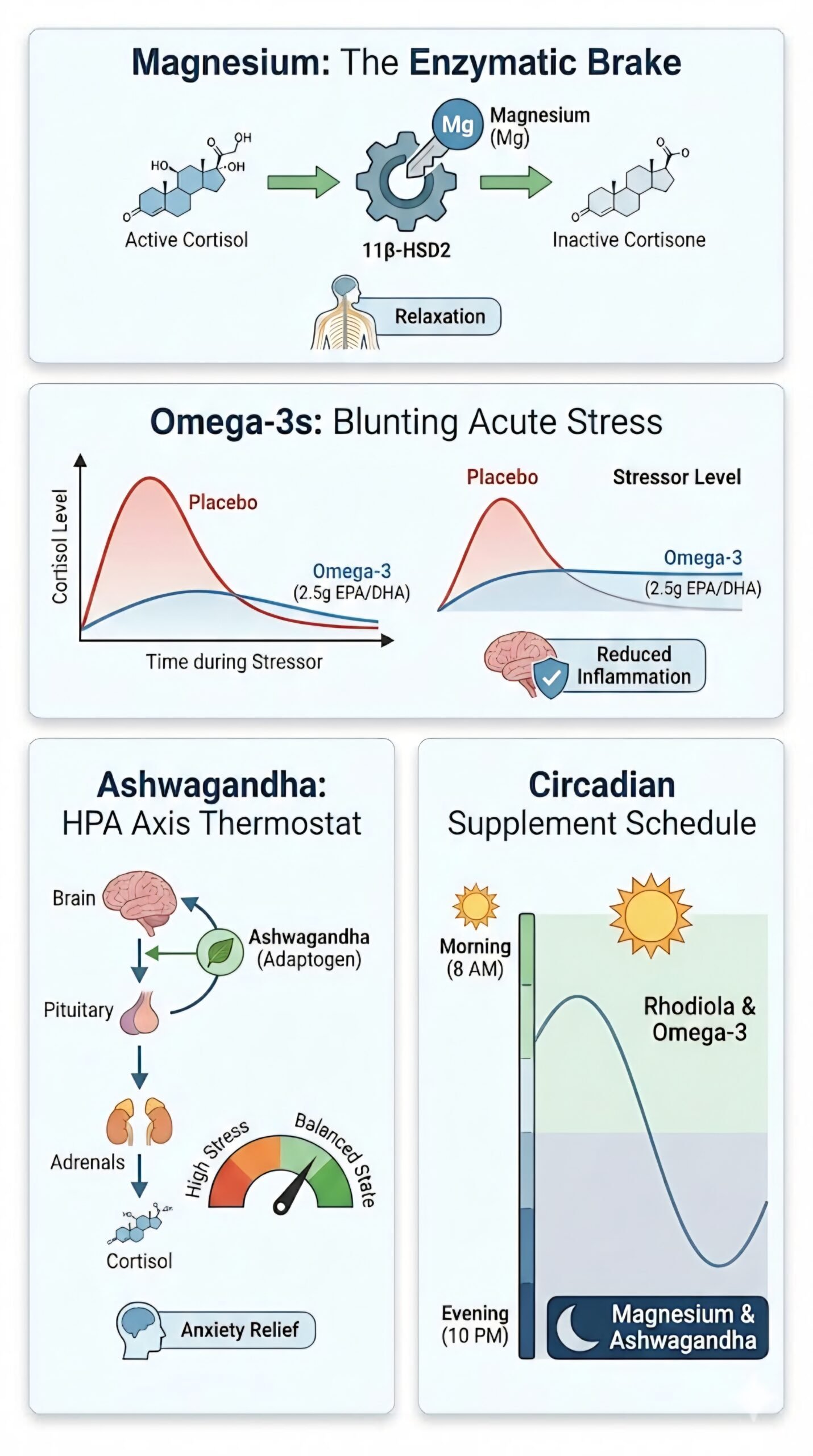
The Adaptogen Powerhouse: Ashwagandha and the HPA Axis “Thermostat”
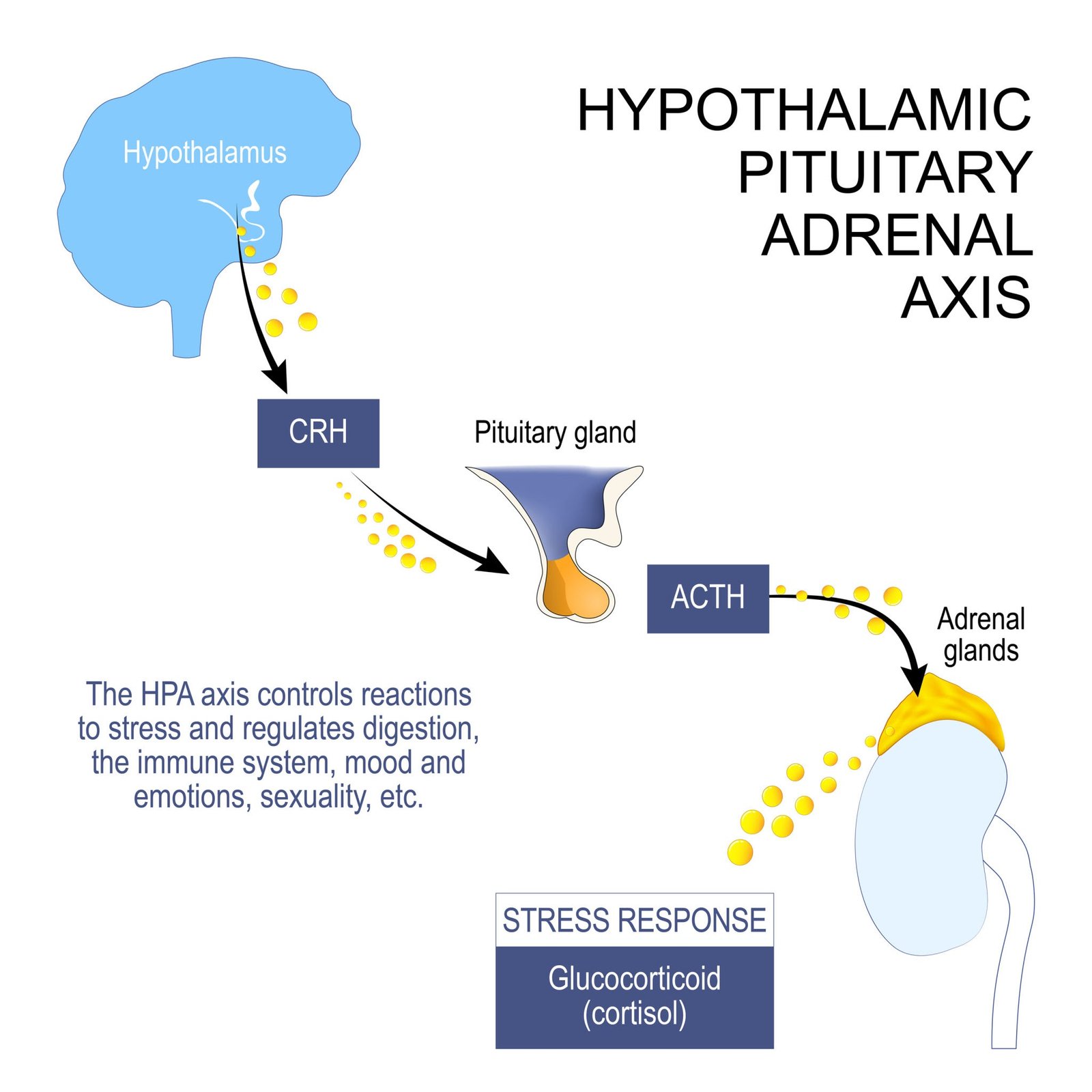
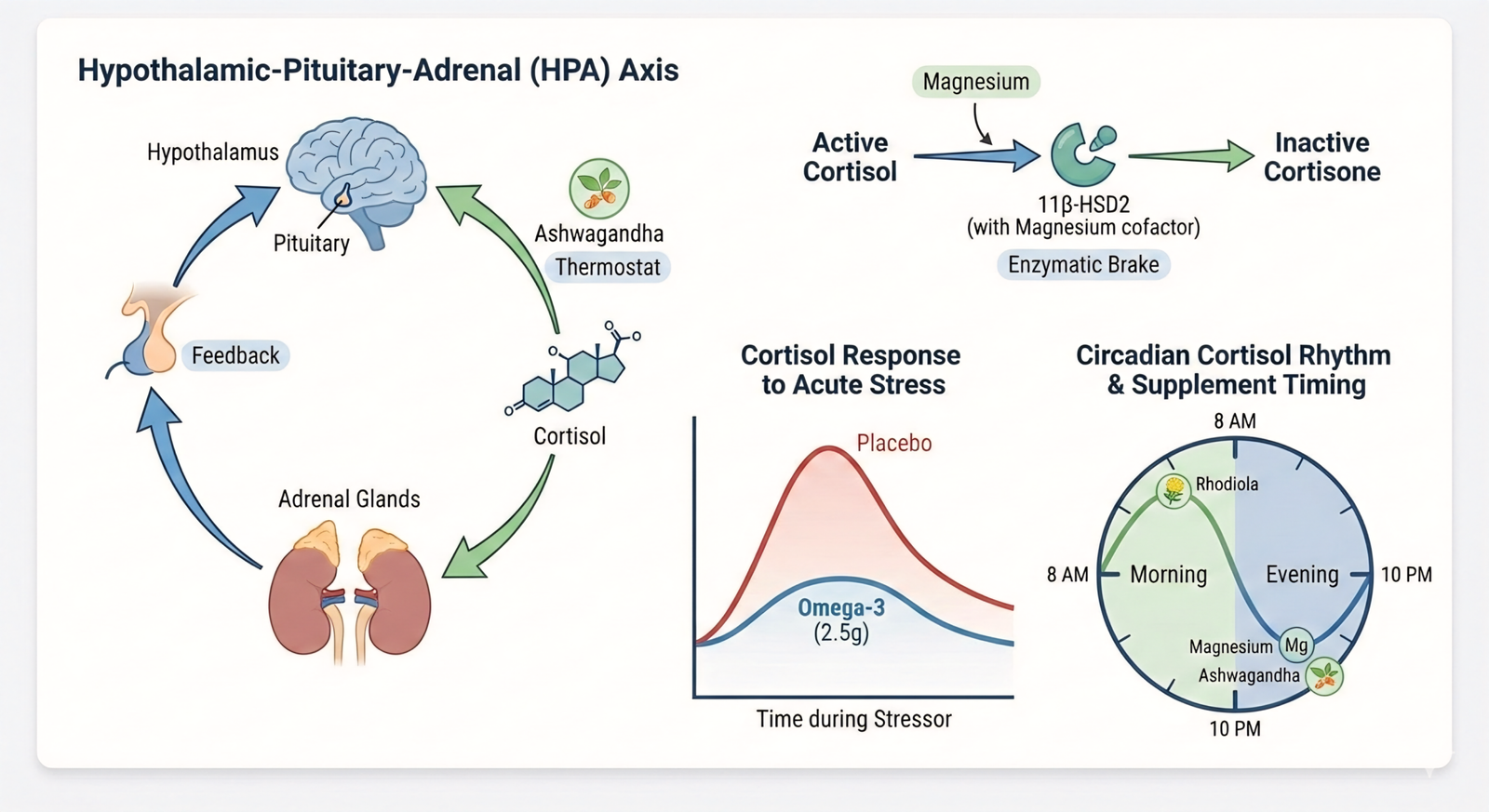
Ashwagandha (Withania somnifera) is not merely a tranquilizer. Its traditional classification as an adaptogen means it helps the body adapt to stress by modulating the hypothalamic-pituitary-adrenal (HPA) axis—the body’s central stress response system. Think of it as recalibrating a sensitive thermostat: during chronic stress, the HPA axis thermostat gets stuck in the “on” position, leading to persistently elevated cortisol. Ashwagandha helps restore its regulatory flexibility.
The clinical evidence is compelling. A systematic review noted that ashwagandha supplementation over 30-112 days was associated with reduced cortisol secretion by 11% to 32.63%. Multiple trials show that doses in the 300-600 mg per day range of a standardized root extract significantly reduce perceived stress and anxiety scores alongside lowering serum cortisol levels. An international task force has provisionally recommended this dose range for managing generalized anxiety disorder.
Choosing Your Extract: KSM-66 vs. Sensoril vs. Shoden
Not all ashwagandha is created equal. The extraction process and plant parts used yield different phytochemical profiles, influencing effects. Here’s a clinical breakdown:
- KSM-66: A full-spectrum root-only extract standardized to 5% withanolides (the key active steroidal lactones). It is the most extensively researched form, with over 20 human clinical trials. Its profile is associated with reducing stress and cortisol while supporting energy and daytime focus, making it ideal for daily resilience without sedation.
- Sensoril: An extract from both root and leaf, standardized to a higher 10% withanolide content. It is often noted for promoting a calming, relaxing effect and has strong research supporting improvements in sleep quality. Effective doses are typically lower (125-250 mg) due to its potency.
- Shoden: A newer, concentrated extract (from root and leaf) with an industry-leading 35% withanolide glycoside concentration. This allows for a very low effective dose (70-200 mg) and is associated with high bioavailability. Early research points to benefits for cognitive health and stress.
Selection Insight: For general daytime stress and HPA axis support, KSM-66’s robust evidence base makes it a premier choice. If stress manifests primarily as evening rumination and sleep difficulty, Sensoril may be more appropriate. Shoden represents a potent, low-dose option.
The Nervous System Brake: Magnesium’s Enzymatic Role
While ashwagandha works on the HPA axis “thermostat,” magnesium acts as a crucial co-factor in the enzymatic machinery that breaks down and clears cortisol from your system. Specifically, magnesium supports the activity of 11β-hydroxysteroid dehydrogenase type 2 (11β-HSD2), an enzyme that converts active cortisol into inactive cortisone in the kidneys.
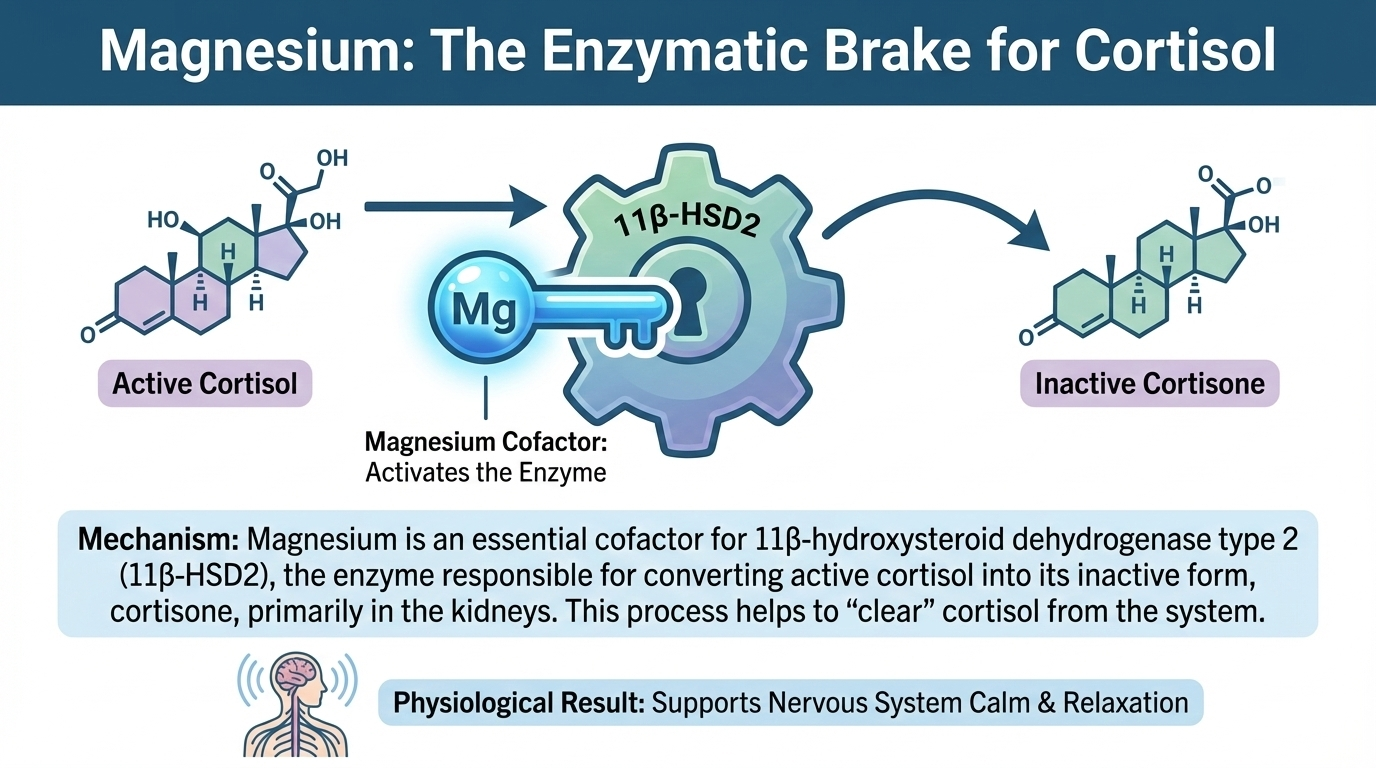
A deficiency in magnesium can impair this deactivation pathway. A 24-week randomized controlled trial provides direct evidence: supplementation with 350 mg of magnesium citrate daily in overweight individuals led to a significant decrease in 24-hour urinary cortisol excretion and an increased activity of the 11β-HSD2 enzyme. This demonstrates magnesium’s role in promoting healthy cortisol metabolism and clearance.
Why Magnesium Glycinate is the Form of Choice
Among the many forms of magnesium, magnesium glycinate (or bisglycinate) stands out for stress and cortisol support for two key reasons:
- Superior Bioavailability and Tolerance: The glycine mineral chelate is highly absorbable and is the least likely to cause the laxative effect associated with forms like magnesium oxide.
- Glycine’s Synergistic Effect: Glycine itself is a calming neurotransmitter. This combination provides the essential magnesium ion alongside a direct supportive nutrient for the nervous system, making it an excellent choice for promoting relaxation without drowsiness.
The effective dose range for stress support is typically 200-400 mg of elemental magnesium from a glycinate form. For most, a dose of 300-350 mg taken in the evening capitalizes on its calming properties to support the natural cortisol decline that should occur at night.
The Anti-Inflammatory Shield: Omega-3 Fatty Acids and Cellular Stress
Chronic stress and elevated cortisol create a pro-inflammatory state, which in turn can dysregulate the HPA axis further. High-dose omega-3 supplementation, specifically the eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA) found in fish oil, intervenes in this cycle by blunting inflammatory and cortisol reactivity to acute stressors.
A pivotal 4-month randomized controlled trial examined this. Sedentary, overweight adults received either 2.5 g/day omega-3, 1.25 g/day omega-3, or a placebo. They then underwent a standardized laboratory stress test. The results were clear:
- The group taking 2.5 g/day of omega-3s had 19% lower overall cortisol output throughout the stress challenge compared to the placebo group.
- This same group also exhibited a 33% reduction in interleukin-6 (IL-6), a key pro-inflammatory cytokine, highlighting the dual anti-cortisol and anti-inflammatory action.
- The lower 1.25 g/day dose showed less pronounced effects, establishing ~2.5 g of combined EPA/DHA as a clinical threshold for significantly modulating the stress response.
Practical Application and Safety
To reach this effective dose, you must look beyond the total “fish oil” content on a label and sum the specific EPA and DHA amounts. A high-quality supplement might provide 1,200-1,500 mg of EPA/DHA per serving, requiring two servings daily.
Safety Note: Doses at or above 2.5 g/day are generally safe but should be discussed with a doctor if you are on blood-thinning medication, due to omega-3’s mild antiplatelet effect. Always choose a reputable brand that molecularly distills its oil and tests for heavy metals and oxidation.
The POLIA Cortisol-Balancing Strategy
The following table synthesizes the protocol data to help you match the right supplement to your primary stress phenotype.
| Supplement | Ideal Form | Clinical Daily Dose | Primary Mechanism | Best For |
|---|---|---|---|---|
| Ashwagandha | KSM-66® Extract | 300-600 mg | HPA axis modulation, adaptogenic | Daytime stress, general HPA axis resilience |
| Ashwagandha | Sensoril® Extract | 125-250 mg | HPA axis modulation, calming | Evening relaxation, stress-related sleep difficulty |
| Magnesium | Glycinate / Bisglycinate | 200-400 mg (elemental) | Cofactor for cortisol metabolism enzymes | Nervous system calm, foundational support, taken nightly |
| Omega-3 Fatty Acids | High-EPA/DHA Triglyceride Form | 2,000-2,500 mg (combined EPA/DHA) | Reduction of stress-induced inflammation | Blunting acute stress reactivity, addressing inflammatory stress |
| Rhodiola Rosea | Extract std. to >3% Rosavins & 1% Salidroside | 200-400 mg (split dose) | Adaptogen, stress-induced fatigue reduction | Mental fatigue, “burnout,” morning energy focus |
Safety, Cycling, and the 12-Week Rule
A responsible protocol is defined not just by what you take, but by how and for how long you take it. This is especially true for adaptogens like ashwagandha.
- The 12-Week Guideline: Most clinical studies on ashwagandha for stress run for 8-12 weeks. The NIH notes that it “appears to be well tolerated for up to about 3 months of use, but its long-term safety is not known”. This establishes a prudent cycle: use for a focused 8-12 week period, then take a break of 2-4 weeks to reassess. This prevents potential tolerance and allows you to evaluate your ongoing need.
- Critical Contraindications: Ashwagandha may stimulate thyroid hormone production and is not recommended for those with hyperthyroidism. Due to its potential immune-modulating effects, individuals with autoimmune diseases should use it with caution and only under medical supervision. It should be avoided during pregnancy. Rare cases of liver irritation have been reported; discontinue use if you experience unusual fatigue, nausea, or jaundice.
- Medical Consultation is Essential: Before starting any high-dose or long-term supplement regimen, consult with your healthcare provider. This is crucial if you have diagnosed health conditions or are taking medications, particularly for thyroid, blood sugar, blood pressure, or anxiety/sleep, due to potential interactions.
2026 Perspective: Circadian Supplementation for HPA Axis Alignment
Modern cortisol management is moving towards chronobiology—aligning interventions with your body’s natural rhythms. Cortisol follows a strong diurnal pattern: a sharp peak 30-45 minutes after waking (the Cortisol Awakening Response), a gradual decline through the day, and a low trough at night. Disruption of this rhythm is a key marker of HPA axis dysfunction.
You can leverage this rhythm through strategic timing:
- Morning (with breakfast): This is the ideal time for supplements that support daytime resilience without sedation. Rhodiola rosea fits here, as it is known to help reduce fatigue and support cognitive performance under stress. A high-quality omega-3 supplement is also well-taken with a morning meal to enhance absorption.
- Evening (with dinner or before bed): This window is for nutrients that support the natural cortisol decline and the body’s transition into recovery mode. Magnesium glycinate is a prime candidate, as its calming properties can support relaxation and sleep onset. For those using ashwagandha for sleep (particularly Sensoril), the evening is the optimal time.
- Ashwagandha Note: If using a full-spectrum extract like KSM-66 for general daytime adaptogenic support, taking it with lunch can be a good compromise—it avoids potential morning drowsiness and allows it to be active during the afternoon stress window.
POLIA Pro-Tip: At POLIA, we recommend tracking your resting heart rate (RHR) and heart rate variability (HRV) via a wearable device. HRV, the variation in time between heartbeats, is a direct indicator of autonomic nervous system balance. Research shows that a larger decrease in HRV during stress anticipation is linked to a higher cortisol response. As your cortisol-balancing protocol takes effect, you may observe a consistent, gradual increase in your HRV (especially overnight) and a decrease in your RHR—objective, biometric confirmation that your nervous system is moving toward greater balance and resilience.
Final Synthesis: A Protocol in Practice
A personalized, evidence-based protocol for someone with high daytime stress and poor sleep recovery might look like this:
- Lifestyle Foundation: Prioritize consistent sleep and mindful morning light exposure to anchor circadian rhythm.
- Morning (with food): Omega-3s (~2.5g EPA/DHA).
- Afternoon (with lunch): Ashwagandha KSM-66 (300mg).
- Evening (with dinner): Magnesium Glycinate (300mg elemental).
- Cycle: Follow this for 12 weeks, then take a 4-week break from ashwagandha, while potentially continuing magnesium and omega-3s. Re-evaluate symptoms and biometrics (like HRV) after the break.
Remember, supplements are adjuncts, not cures. Their greatest power is unlocked when they are part of a holistic strategy that addresses sleep, nutrition, movement, and mindset. By applying these principles with precision and patience, you can move beyond simply managing stress symptoms and toward fundamentally recalibrating your body’s resilience.